"Cut the games, not the care."
"Cut the games, not the care".
Every dollar in health care goes somewhere. Right now far too many dollars go to forms, code battles, and scams instead of stitches and pills.
Walk into any clinic and count the number of people who never touch a patient. They code visits, chase claims, and argue with insurers. Every insurer has different rules and different ways to deny, delay, and downcode. That cost is not theoretical. It is baked into every premium and every bill.
SAFECARE cuts that waste in two steps.
First: Unify the Payment Stream
It unifies the payment stream. One main payer for essential care. One set of rules. One set of codes. Clinics still need billing staff, but not to run a daily war against twenty payers with twenty playbooks.
Fraud: Second, Treat Fraud Like a Felony
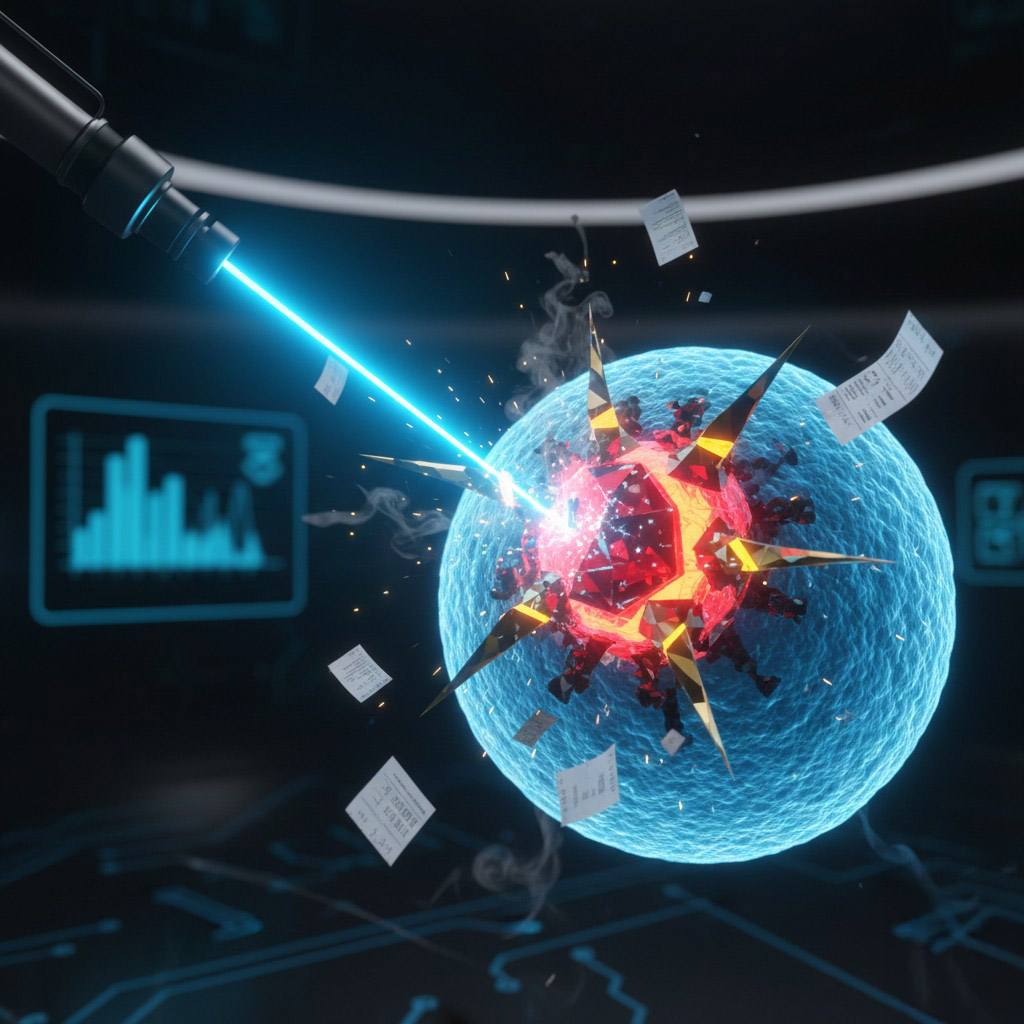
It treats fraud like a high level crime, not a cost of doing business. All claims flow through one national platform that can see patterns no single payer can see. This is where modern AI earns its keep. Not because it is "smart", but because it can scan millions of transactions and find statistical fingerprints humans miss.
- A provider billing more hours than exist in a day.
- A clinic that suddenly "discovers" an epidemic of the same high-cost procedure.
- A network that repeats the same diagnosis and the same expensive drug pattern across thousands of claims.
These are not gut feelings. They are pattern anomalies.
Real World Comparison
This is not theoretical either. TSA already uses advanced screening systems where scanners generate 3-D images of bags and apply automated detection algorithms to identify threats in carry-on and checked baggage. TSA describes CT screening as applying "sophisticated algorithms" to detect explosives and improve threat detection. DHS also lists TSA use cases that include AI and machine learning efforts to automate detection of prohibited items. The key point is the workflow. The system flags what looks wrong at scale, then humans decide what happens next.
SAFECARE uses the same discipline. Algorithms flag suspicious claims before money leaves the system, but human review makes the call. Providers and members get clear explanations and due process through appeals. The goal is accuracy, not automated denial.
Summary: Bottom Line
When real fraud clears a clear threshold, it becomes a federal felony with mandatory penalties and asset seizure. The message is simple. We would rather pay for nurses than shell companies. We would rather fund mental health care than buy fake back braces and nonexistent tests. This is how you defend a public system. You do not starve patients. You starve the parasites.